COVID-19’s silent impact extends to neurological and cardiac health
The study makes clear that COVID-19 cannot be treated as a short-term respiratory illness. Instead, health systems must plan for the long haul. The authors argue for integrated, multidisciplinary care that spans pulmonology, cardiology, neurology, nephrology, and beyond. Rehabilitation and monitoring should extend months or even years after acute infection, especially for high-risk groups.
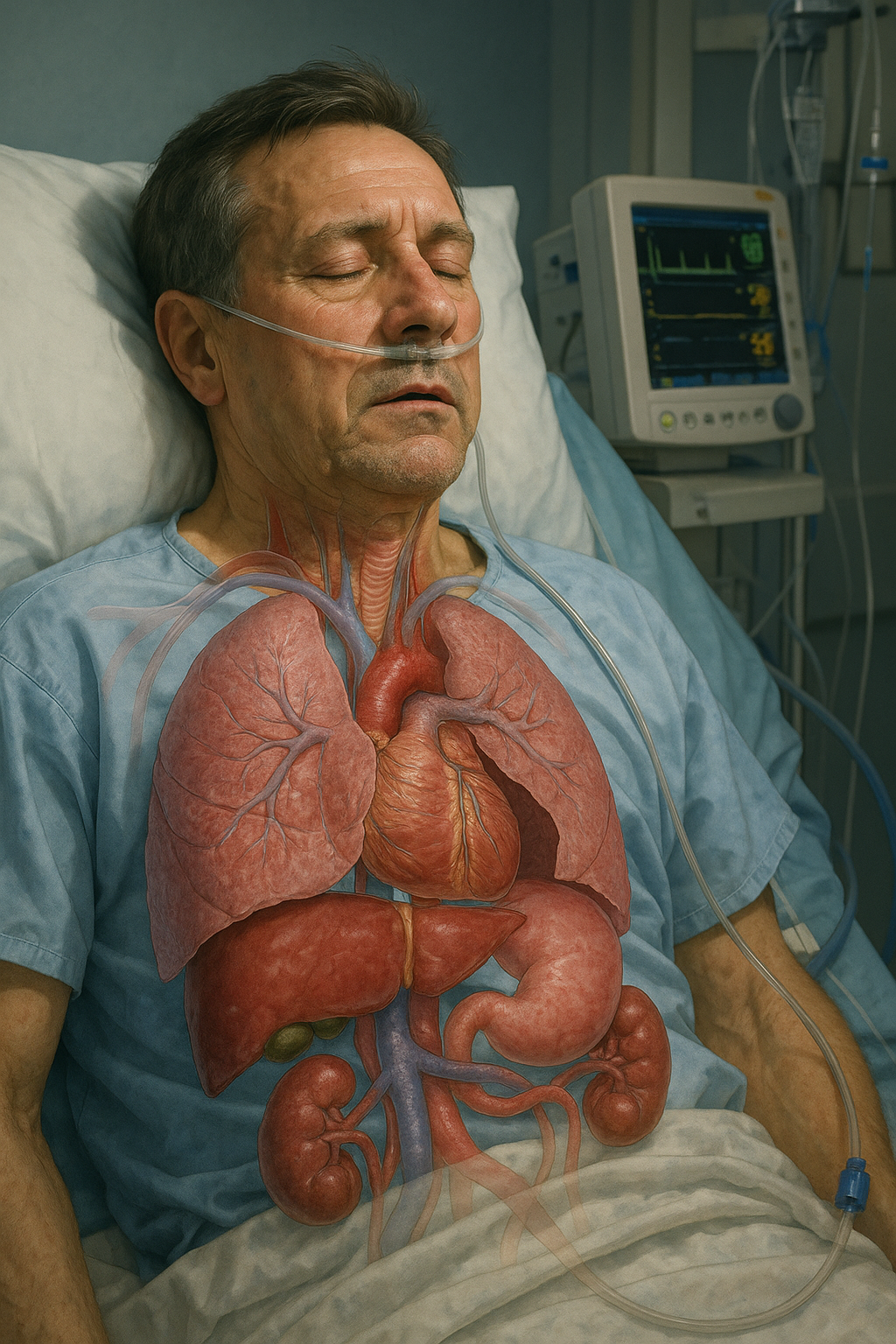
A new review has revealed that COVID-19’s impact extends far beyond the lungs, leaving lasting damage across multiple organ systems. The study, Silent Invasion: COVID-19’s Hidden Damage to Human Organs, published in COVID, brings together findings from more than 160 peer-reviewed studies and over two million patients.
The international team of authors warns that the pandemic should no longer be viewed narrowly as a respiratory crisis but as a systemic disease with long-term consequences.
How widespread is COVID-19’s multi-organ impact?
The researchers found that multi-organ involvement was common during the acute phase of infection. In hospitalized patients, lung complications remained the most frequent, affecting more than three-quarters of cases. Yet nearly half of patients experienced neurological issues, while cardiovascular and kidney problems also appeared at significant rates.
The review highlights that these problems are not confined to the initial infection. Between 10 and 35 percent of patients showed evidence of persistent organ dysfunction six months later, underscoring the scale of what has come to be known as long COVID.
The findings extend beyond the major systems. Reports of reproductive changes, such as reduced testosterone levels in men and menstrual disruptions in women, suggest that COVID-19’s reach is more extensive than many clinicians initially understood. Skin manifestations, from rashes to vascular complications, were also tied to poorer outcomes in several studies.
What mechanisms drive lasting organ damage?
The authors identified three recurring processes behind COVID-19’s multi-organ impact: cytokine storm, endothelial dysfunction, and microvascular thrombosis. Together, these mechanisms explain how a virus that enters primarily through the respiratory tract can unleash widespread systemic harm.
Cytokine storm, marked by extreme immune overactivation, was recorded in the majority of severe cases. Endothelial dysfunction, which disrupts the lining of blood vessels, appeared in nearly nine out of ten patients studied. Microvascular thrombosis, or small blood clots, was detected in close to half. These mechanisms combined to create cascading effects across the brain, heart, kidneys, and other organs.
Importantly, the severity and type of organ involvement varied with viral variants. The Delta wave produced more severe lower-respiratory complications, while Omicron was linked with upper-airway infections, particularly among vaccinated groups. Neurological complaints, although still common, were somewhat reduced in Omicron compared to earlier variants. These differences underline the need for ongoing monitoring as the virus continues to evolve.
What do the findings mean for healthcare systems?
The study makes clear that COVID-19 cannot be treated as a short-term respiratory illness. Instead, health systems must plan for the long haul. The authors argue for integrated, multidisciplinary care that spans pulmonology, cardiology, neurology, nephrology, and beyond. Rehabilitation and monitoring should extend months or even years after acute infection, especially for high-risk groups.
They also highlight the importance of long-term surveillance programs. By tracking outcomes across large populations, governments and healthcare providers can better understand the prevalence of long COVID and allocate resources accordingly. The review warns that without such programs, many patients with lingering organ dysfunction risk being overlooked or misdiagnosed.
Finally, the study highlights the need for research that targets the shared mechanisms driving organ damage. Treatments that address cytokine storm, endothelial health, and microvascular clotting could provide cross-cutting benefits across organ systems. Rather than siloed approaches, the authors call for therapies and monitoring strategies designed with systemic impact in mind.
- FIRST PUBLISHED IN:
- Devdiscourse










