Chatham Islands Celebrate Launch of Permanent Ultrasound Services in Rural Health
The Chatham Islands project is seen as a proof of concept for how remote diagnostic technology can transform access to care in isolated communities.
- Country:
- New Zealand
Residents of the Chatham Islands now have access to permanent ultrasound services for the first time, marking a major advancement in rural healthcare and diagnostic access. The milestone was announced by Health Minister Simeon Brown, who described it as a “transformational step” toward ensuring all New Zealanders—no matter how remote—can receive timely, high-quality medical care close to home.
A Breakthrough for Rural and Island Healthcare
Until now, Chatham Islands residents faced significant barriers to receiving even basic diagnostic imaging. The absence of local ultrasound capability meant patients were often required to travel hundreds of kilometres to the mainland, typically to Christchurch or Wellington, for routine scans. Such travel often involved long waiting times, weather-dependent flights, and major expenses for both patients and the health system.
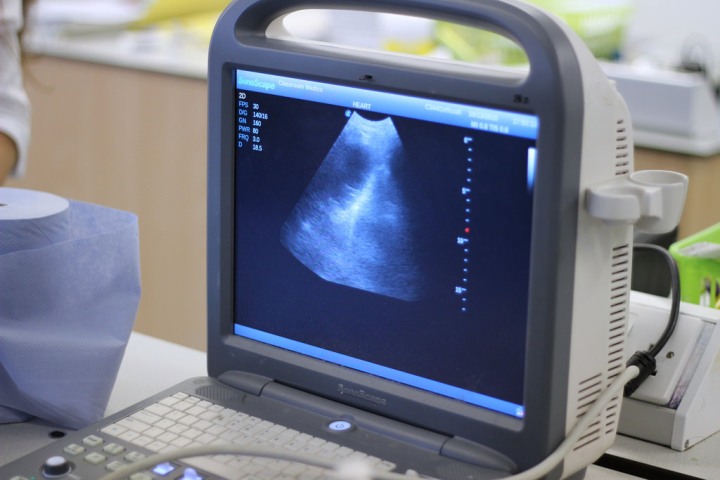
The introduction of the new ultrasound service at the Chatham Islands Health Centre changes that reality. For the first time, locals can access on-island diagnostic imaging for a wide range of health conditions, including gallstones, bladder problems, deep vein thrombosis (DVT), and soft tissue injuries.
“This is a significant milestone for the Chatham Islands community, improving access to both routine and emergency diagnostic care,” said Minister Brown. “It brings care closer to home, reduces the need for travel, and ensures patients receive the same standard of service as those on the mainland.”
Innovative Technology and Remote Collaboration
The service uses advanced tele-ultrasound technology that allows local healthcare staff to perform scans under remote guidance from trained sonographers and specialists at Christchurch Hospital. Through secure video connections, experts can view images in real time, guide scanning techniques, and provide immediate clinical feedback.
In urgent or emergency situations, live streaming of scan images to Christchurch enables intensive care and radiology teams to confirm diagnoses and prepare for potential patient transfers before they leave the islands. This ensures continuity of care and more efficient treatment planning, saving valuable time when minutes matter.
A successful live trial of the system was conducted this week, with Christchurch-based ICU and radiology teams participating remotely in a simulated clinical environment. The trial demonstrated the system’s reliability and clinical effectiveness, paving the way for full-scale deployment.
Supporting Specialists and Expanding Services
Minister Brown noted that the new system will not only improve outcomes for patients but also support visiting specialists—including general practitioners, radiologists, and emergency care teams—who travel periodically to the islands. The availability of on-site imaging will allow them to deliver more comprehensive and immediate care during their visits.
The Health Centre plans to expand the range of ultrasound services as local staff gain further training and experience. This will eventually include maternity and antenatal scans, giving expectant mothers the ability to receive important pregnancy monitoring without leaving their community.
“This initiative reflects our commitment to strengthening rural health services,” Brown said. “By combining technology, training, and teamwork, we’re creating sustainable models of care that work for even the most remote regions of New Zealand.”
Reducing Costs and Improving Access
The Ministry of Health estimates that the new service will significantly reduce patient travel costs and the associated logistical challenges for families and healthcare providers. It will also decrease waiting times for diagnostic imaging, ensuring earlier detection and management of conditions that might otherwise worsen before treatment.
Health officials say this initiative aligns with the Government’s broader Rural Health Strategy, which aims to bridge the urban-rural gap in healthcare outcomes through digital innovation and workforce support.
A Model for Other Remote Communities
The Chatham Islands project is seen as a proof of concept for how remote diagnostic technology can transform access to care in isolated communities. If successful, similar tele-ultrasound systems could be rolled out in other rural and maritime regions, including parts of the West Coast, Northland, and the East Cape.
Minister Brown said the initiative was “a perfect example of technology working hand in hand with people.”
“This is what modern healthcare should look like—smart, connected, and equitable,” he said. “Every New Zealander, whether they live in Auckland or the Chatham Islands, deserves access to quality care.”
The permanent ultrasound service is expected to be fully operational within the coming months, with staff training continuing throughout the year.










