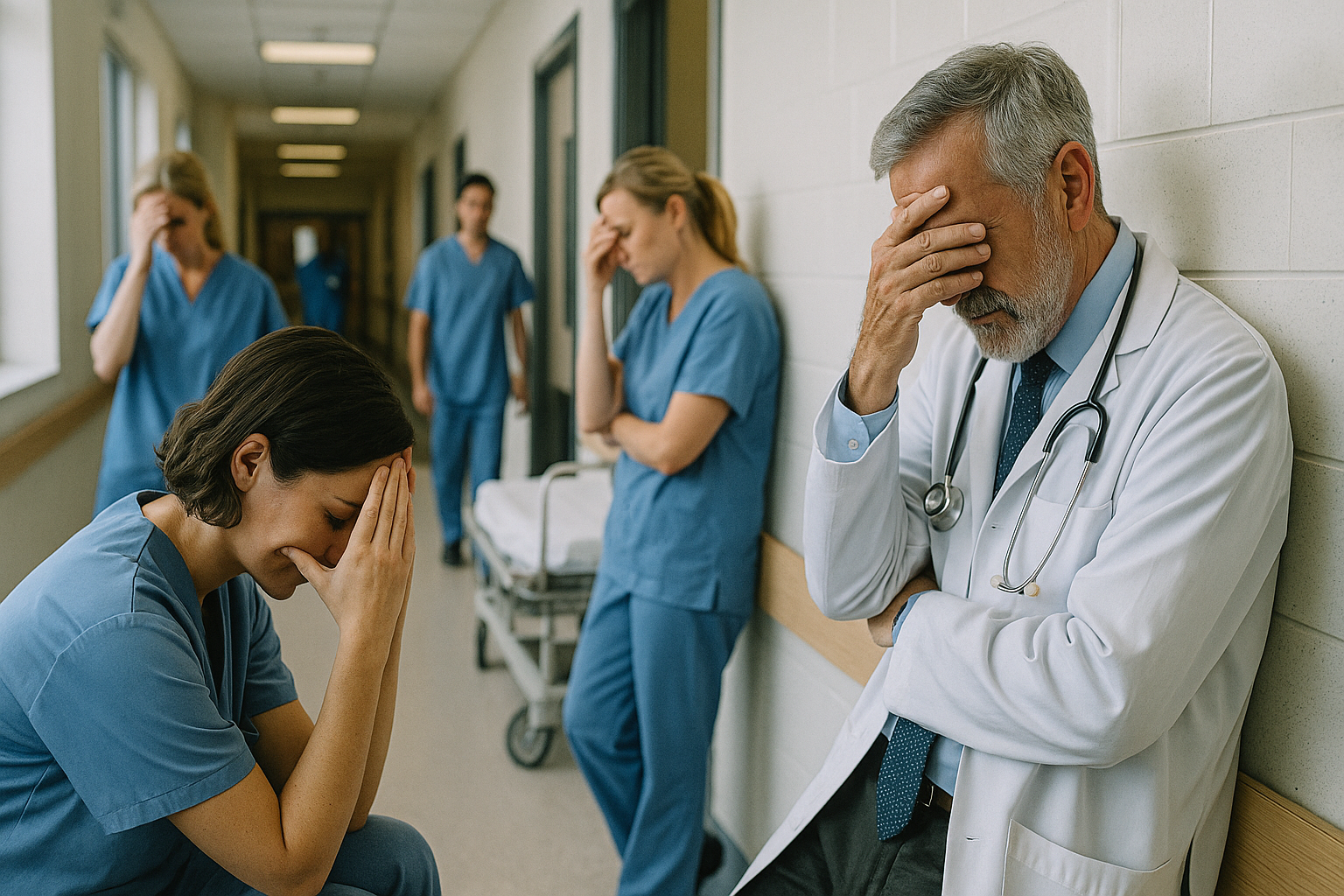
Caring under pressure: WHO reveals mental toll on Europe’s doctors and nurses
A new WHO report reveals a mental health crisis among Europe’s doctors and nurses, with high levels of burnout, anxiety, and depression across the region. It urges urgent reforms to protect healthcare workers, warning that the survival of health systems depends on caring for those who care for others.
The mental health of Europe’s doctors and nurses has reached alarming levels, according to a new report by the World Health Organization (WHO) in collaboration with the European Observatory on Health Systems and Policies, the European Commission’s Directorate-General for Health and Food Safety (DG SANTE), and the University of Bergen. The report, Mental Health of Nurses and Doctors: Findings from a Survey in the European Union, Iceland, and Norway, provides one of the most detailed portraits yet of how exhaustion, anxiety, and burnout have taken hold across Europe’s health workforce.
A Workforce on the Edge
Based on a survey conducted between 2023 and 2024 across the European Union, Iceland, and Norway, the study gathered responses from thousands of doctors and nurses in both public and private sectors. The results reveal a troubling picture: almost half of all nurses and more than one-third of doctors reported symptoms consistent with anxiety or depression. Around 60 percent of nurses said they felt emotionally exhausted “most or all of the time.”
The report warns that burnout has become “endemic”, no longer an exception but a routine part of working life. Many healthcare workers continue to log long shifts that far exceed the EU’s legal limit of 48 hours a week, often without adequate rest or access to counselling. The culture of endurance, once seen as a badge of dedication, has turned into a silent epidemic of despair. One nurse from southern Europe summed up the feeling shared by many: “We are expected to care for everyone else, but no one cares for us.”
Where You Work Matters
The survey found wide variations in mental health depending on geography and working conditions. Southern and Eastern European countries reported the highest levels of stress and burnout, closely linked to staff shortages, limited resources, and underfunded health systems. By contrast, Nordic and Western European nations fared somewhat better thanks to stronger workplace protections and more accessible mental health support.
However, even in better-performing regions, high workloads and administrative burdens continue to weigh heavily on staff morale. Nurses consistently reported higher levels of exhaustion and job dissatisfaction than doctors, reflecting deeper inequalities in pay, recognition, and professional autonomy. The WHO notes that these disparities undermine the cohesion of the health workforce and make retention even more difficult in already strained systems.
Women and Young Professionals Hit Hardest
Gender and age also play significant roles in this mental health crisis. Women, who make up the majority of Europe’s nursing workforce and a growing proportion of doctors, were far more likely to report symptoms of anxiety and emotional strain than men. The pressures of balancing professional responsibilities with family and social expectations compound their stress.
Younger doctors and nurses were found to be especially vulnerable. Many spoke of “moral injury”, the anguish of being unable to provide patients with the level of care they know is needed because of resource constraints or staff shortages. This moral distress is pushing some early-career professionals to consider leaving medicine altogether, threatening the sustainability of the region’s healthcare systems.
Institutions Failing Their Own Caregivers
The WHO report highlights a striking lack of institutional support for healthcare workers’ mental well-being. Fewer than one in three respondents said their workplace offered confidential psychological services, and even fewer felt comfortable using them. Fear of stigma or professional repercussions remains widespread.
The report makes it clear: mental distress among health workers is not a personal weakness but a systemic failure. Long hours, chronic understaffing, low pay, and limited career progression are structural problems that demand structural solutions. Short-term wellness initiatives or occasional appreciation campaigns, the report warns, are not enough. What is needed is a fundamental rethinking of how health systems value and protect their workforce.
A Call for Urgent Reform
To address this crisis, WHO and its research partners urge European governments to act decisively. Their recommendations include integrating mental health services into occupational health care, developing national strategies for workforce well-being, and ensuring that data on burnout and psychological distress are regularly collected and publicly reported. Hospitals should offer confidential, stigma-free support services and create safe spaces for staff to speak openly about their mental health challenges.
Strong leadership is essential. The report finds that hospitals where staff feel heard and respected tend to have lower burnout rates. A model introduced in the report, the “well-being ecosystem”, identifies four key pillars for protecting healthcare workers’ mental health: fair pay, adequate staffing, supportive management, and a culture of compassion.
The WHO concludes with a clear warning: the mental health of doctors and nurses is not just a personal issue; it is a matter of public health and system survival. Without decisive action, Europe risks losing the people who keep its hospitals running.
“Caring for those who care for others must be treated as a political and moral priority,” the report states. Behind every statistic lies a story of sacrifice and fatigue, of professionals who have held up Europe’s health systems through some of the hardest years in modern history. The message is unmistakable: the future resilience of healthcare in Europe will depend not only on funding or technology but on restoring dignity, empathy, and psychological safety to the people at its heart.
- FIRST PUBLISHED IN:
- Devdiscourse
ALSO READ
WHO Warns One in Six Infections Now Resistant to Antibiotics Worldwide
WHO Launches EIOS 2.0 to Strengthen Global Early Warning Against Health Threats
Revolutionizing TB Care: New WHO Guidelines Combat Undernutrition
The Man Who 'Died' to Escape Justice: Virender Vimal's Extraordinary Evasion
Access to Medicines Still Uneven in South-East Asia, Finds WHO Regional Report










